
Dysphagia or difficulty swallowing is a common problem that can happen at any stage of Parkinson’s and is described as difficulty moving food, liquid, saliva or medication from your mouth to your stomach. Eating and drinking can be uncomfortable, stressful and even dangerous if you have dysphagia. If not managed properly life-threatening medical problems such as pneumonia, choking, poor nutrition and dehydration can occur. Early detection and individualised treatment of dysphagia is crucial to prevent complications and improve your quality of life.
Signs and symptoms of dysphagia
Signs and symptoms of dysphagia can range from mild to severe. If you think you or a loved one might have a swallowing problem, it is important to get professional help as soon as possible. Speech Pathologists are experts in dysphagia and can assess your swallowing ability and safety. Seek help from your doctor and a Speech Pathologist if you notice any of the following signs or symptoms:
- A feeling that food or drink gets stuck in your throat
- A feeling that food or drink is going the wrong way
- Long mealtimes or eating slowly (it takes >30 minutes to finish a meal)
- Coughing, choking or frequent throat clearing during or after eating and drinking
- Becoming short of breath or your breathing changes when eating and drinking
- Avoiding certain foods because they are difficult to swallow
- Unplanned weight loss, or failing to put on weight because of avoiding foods or finding it hard to eat
- Frequent chest infections with no known cause
Treatment of dysphagia
Management of your dysphagia should be based on results of a comprehensive assessment by a Speech Pathologist. By determining the cause and severity of your dysphagia, a Speech Pathologist can recommend a number of compensatory techniques and exercises for safe swallowing which may include:
- Diet and fluid modifications
- Use of specific equipment/utensils to facilitate swallow function
- Postural/position techniques
- Pacing and feeding strategies
- Oral-motor therapy/exercises
- Swallowing manoeuvres
- Sensory stimulation
If your swallowing problem is very severe, a Speech Pathologist may recommend taking food and liquid via a tube that goes directly to your stomach.
Diet and fluid modifications for dysphagia
Depending on your level of dysphagia your Speech Pathologist may suggest foods be chopped, minced or pureed and liquids thickened. The International Dysphagia Diet Framework, shown below, outlines the different types of food textures and liquid categories that may be suggested. The framework was developed to provide standardised terminology and definitions to describe food textures and liquid thickness.
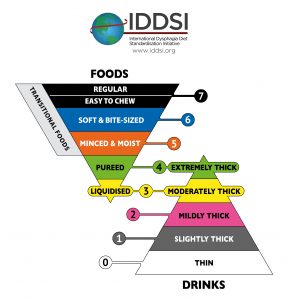
Below is a brief summary of some of the common texture modified diets and thickened liquids that may be suggested for people with Parkinson’s who have dysphagia. For detailed information on the different food and drink categories as well as testing methods that help ensure consistent production of prescribed foods and liquids visit iddsi.org
Dysphagia and texture modified diets – FOR ADULTS
Pureed diet

Pureed food has a smooth texture with no lumps, does not require chewing and is usually eaten with a spoon. Pureed food should not be sticky, and no thin liquid should separate from the food. It is safest to test pureed food using the IDDSI Fork Drip Test and IDDSI Spoon Tilt Test.
Minced and Moist diet

Minced and moist food looks like puree but with small soft lumps no bigger than 4mm x 4mm x 15mm in size. This category of food requires minimal chewing and can be eaten with a fork or spoon. Lumps can be easily mashed with just a little pressure from a fork and are easy to squash with your tongue. Minced and moist food should not be sticky, and no thin liquid should separate from the food. It is safest to test minced and moist food using the IDDSI Fork Drip Test and IDDSI Spoon Tilt Test.

Soft and Bite-Sized diet

Soft and bite-sized food is soft, tender and moist throughout with no separate thin liquid present. Food piece sizes are designed to minimise choking risk and should be no bigger than 1.5cm x 1.5cm in size. Food pieces can be mashed/broken down with pressure from a fork, a spoon or chopsticks. The ability to chew bite-sized pieces down into little pieces that are safe to swallow is required. It is safest to test soft and bite-sized food using the IDDSI Fork Pressure Test.

Easy to Chew diet

Easy to chew food is normal everyday food of soft/tender texture. Food piece size is not restricted so foods may be a range of sizes. The ability to “bite-off” pieces of food safely and chew bite-sized pieces down into little pieces that are safe to swallow is required. Foods that are hard, tough, chewy, fibrous, have stringy textures, pips/seeds, bones or gristle are not recommended. Easy to chew food should break apart easily using the side of a fork or spoon. It is safest to test easy to chew food using the IDDSI Fork Pressure Test.
Easy to chew foods are not intended for people where there is an identified increased risk of choking. People who are unsafe to eat without supervision are also not considered suitable for these foods.
Mixed or dual consistency foods
Mixed or dual consistency foods are more challenging to swallow and are not recommended for people with dysphagia. Examples of mixed or dual consistency foods include chicken noodle soup, breakfast cereal with milk and watermelon which appears to be a single consistency on a plate but may quickly separate into two consistencies in your mouth.
An easy to chew diet may include mixed or dual consistency foods if your Speech Pathologist has approved this.
What about bread?
Bread is considered a choking risk and is not permitted on an easy to chew, soft and bite-sized, minced and moist or pureed diet. Although bread looks and feels soft, it cannot be easily mashed or broken down due to its fibrous nature.
Swallowing medications
Ability to swallow whole pills, tablets and capsules can be assessed on a case-by-case basis by a Speech Pathologist. If you are unable to swallow whole pills, tablets or capsules consult your Doctor for advice on alternative formulations.
Dysphagia and thickened liquids – FOR ADULTS
Mildly Thick
Mildly thick liquids may be recommended if thin liquids flow too fast to be controlled safely. Mildly thick liquids flow at a slightly slower rate and can be consumed using a straw or from a standard cup. It is safest to measure mildly thick liquids using the IDDSI Flow Test.
Moderately Thick

Moderately thick liquids may be recommended if your tongue control is not good enough to manage mildly thick or thin liquids. This level of thickness allows more time for oral control and can be consumed from a cup or eaten with a spoon. It is safest to measure moderately thick liquids using the IDDSI Flow Test and IDDSI Fork Drip Test.
Extremely Thick

Extremely thick liquids may be recommended if your tongue control is not good enough to manage moderately thick, mildly thick or thin liquids. Extremely thick liquids cannot be sucked through a straw or drunk from a cup and should be eaten with a spoon. It is safest to measure extremely thick liquids using the IDDSI Fork Drip Test and IDDSI Spoon Tilt Test.
Thickened liquids should be tested at the intended serving temperature as generally speaking, a thickened liquid that is served cold/chilled will be thicker than if it is served at room temperature, or heated.
A range of thickening products and pre-thickened ready-to-drink liquids are available commercially. Foods such as jelly and ice-cream melt in your mouth and become a thin liquid so should be avoided if thickened liquids have been prescribed for you.
Final thoughts
Dysphagia is a common problem that can happen at any stage of Parkinson’s. If you think you or a loved one might have a swallowing problem, seek professional help as soon as possible. Early detection and individualised treatment of dysphagia is crucial to help prevent complications and improve your quality of life. As part of your treatment plan a texture modified diet or thickened liquids may be suggested along with compensatory techniques and exercises for safe swallowing.
This article is intended as general information only. Swallowing is a complex process and treatment of dysphagia is not one-size fits all. Always consult your doctor and a Speech Pathologist for specific advice on your needs.
Sources
-
Cichero, J.A.Y., Steele, C., Duivestein, J. et al. The Need for International Terminology and Definitions for Texture-Modified Foods and Thickened Liquids Used in Dysphagia Management: Foundations of a Global Initiative, Curr Phys Med Rehabil Rep (2013) 1: 280
-
Speech Pathology Australia, Swallowing – fact sheet.
-
Miseon Kwon, Jae-Hong Lee, J Mov Disord 2019; 12(3): 152-160, Published online: September 30, 2019, Oro-Pharyngeal Dysphagia in Parkinson’s Disease and Related Movement Disorders
-
The American Speech-Language-Hearing Association (ASHA), Adult Dysphagia – Clinical topic.
-
The International Dysphagia Diet Standardisation Initiative, 2016. Including the following documents: Complete IDDSI Framework Detailed definitions, IDDSI Framework Testing Methods, Resources, FAQ
Parkinson Diet – Terms & conditions / Privacy policy


